Mammograms are, to date, the best diagnostic test we have to catch breast cancer and other breast conditions. If you’re like most women, you probably have a few questions about the testing guidelines and what to expect when mammogram time comes around. Here, we walk through some of the most important details of this screening.
“I don’t need a mammogram; I have no family history!”
We need to address this misconception first. If you are a woman, you have a risk of breast cancer. According to statistics, 1 in 8 women with no family history is at risk of breast cancer. Due to the sheer number of breast cancer diagnoses, statistics suggest that more of the annual cases of breast cancer affect women without a family history than women who do have this risk factor.
Mammogram Timing
Guidelines for mammogram screening have changed from time to time so, it is no wonder why women struggle knowing when and how often they should get this screening. women with an AVERAGE risk of breast cancer schedule mammograms every year beginning at age 40. There is no specific age to stop this screening. This is determined by the patient’s overall health.
Mammogram scheduling may also have to consider insurance coverage. Most insurance companies require subscribers to schedule mammograms at least 366 days apart. Each woman should check with her insurance company and then mark her calendar accordingly. Also, because it may be necessary to return to the center or a doctor’s office for further testing, women are encouraged to schedule mammograms when they will be in town for at least two weeks following their screening.
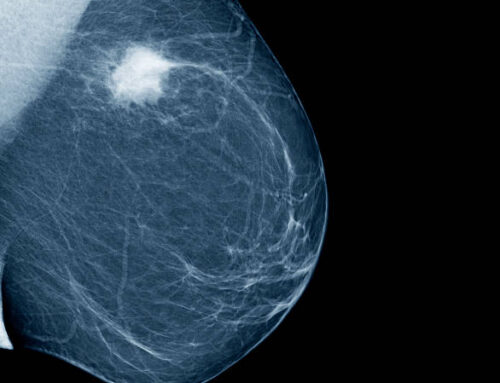
2D vs 3D Mammogram
A conventional 2D mammogram compresses the breast in two positions, producing 2 images of each. In these images, cancer can look similar to normal glandular breast tissue. The positioning and imaging of 2D mammography could miss cancer hidden within dense breast glands. A 3-dimensional mammogram uses the same two positions for imaging as a 2D mammogram. However, 4 images of each breast are produced, not 2. Two of the images produced are 2D and two are 3D. This technique is better at distinguishing small cancerous growths from normal breast tissue, reducing the likelihood of being called back for further screenings.
American Cancer Society Recommendations for the Early Detection of Breast Cancer
Finding breast cancer early and getting state-of-the-art cancer treatment are two of the most important strategies for preventing deaths from breast cancer. Breast cancer that’s found early, when it’s small and has not spread, is easier to treat successfully. Getting regular screening tests is the most reliable way to find breast cancer early. The American Cancer Society has screening guidelines for women at average risk of breast cancer, and for those at high risk for breast cancer.
What are screening tests?
Screening refers to tests and exams used to find a disease in people who don’t have any symptoms. The goal of screening tests for breast cancer is to find it early, before it causes symptoms (like a lump in the breast that can be felt). Early detection means finding and diagnosing a disease earlier than if you’d waited for symptoms to start.
Breast cancers found during screening exams are more likely to be smaller and less likely to have spread outside the breast. The size of a breast cancer and how far it has spread are some of the most important factors in predicting the prognosis (outlook) of a woman with this disease.

American Cancer Society screening recommendations for women at average breast cancer risk
The COVID-19 pandemic has resulted in many non-emergency procedures being put on hold. This has led to a substantial decline in cancer screening. Health care facilities are providing cancer screening during the pandemic with many safety precautions in place. Learn how you can talk to your doctor and what steps you can take to plan, schedule, and get your regular cancer screenings in Cancer Screening During the COVID-19 Pandemic.
These guidelines are for women at average risk for breast cancer. For screening purposes, a woman is considered to be at average risk if she doesn’t have a personal history of breast cancer, a strong family history of breast cancer, or a genetic mutation known to increase risk of breast cancer (such as in a BRCA gene), and has not had chest radiation therapy before the age of 30. (See below for guidelines for women at high risk.)
- Women between 40 and 44 have the option to start screening with a mammogram every year.
- Women 45 to 54 should get mammograms every year.
- Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms. Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
- All women should understand what to expect when getting a mammogram for breast cancer screening – what the test can and cannot do.
Clinical breast exams are not recommended for breast cancer screening among average-risk women at any age.
Mammograms
Mammograms are low-dose x-rays of the breast. Regular mammograms can help find breast cancer at an early stage, when treatment is most likely to be successful. A mammogram can often find breast changes that could be cancer years before physical symptoms develop. Results from many decades of research clearly show that women who have regular mammograms are more likely to have breast cancer found earlier, are less likely to need aggressive treatments like surgery to remove the entire breast (mastectomy) and chemotherapy, and are more likely to be cured.
Mammograms are not perfect. They miss some breast cancers. And if something is found on a screening mammogram, a woman will likely need other tests (such as more mammograms or a breast ultrasound) to find out if it is cancer. There’s also a small chance of being diagnosed with a cancer that never would have caused any problems had it not been found during screening. (This is called overdiagnosis.) It’s important that women getting mammograms know what to expect and understand the benefits and limitations of screening.
2D vs. 3D mammograms
In recent years, a newer type of mammogram called digital breast tomosynthesis (commonly known as three-dimensional [3D] mammography) has become much more common, although it’s not available in all breast imaging centers.
Many studies have found that 3D mammography appears to lower the chance of being called back after screening for follow-up testing. It also appears to find more breast cancers, and several studies have shown it can be helpful in women with more dense breasts. A large study is now in progress to better compare outcomes between 3D mammograms and standard (2D) mammograms.
It should be noted that 3D mammograms often cost more than 2D mammograms, and this added cost may not be covered by insurance.
The American Cancer Society (ACS) breast cancer screening guidelines consider having had either a 2D or 3D mammogram as being in line with current screening recommendations. The ACS also believes that women should be able to choose between 2D and 3D mammography if they or their doctor believes one would be more appropriate, and that out-of-pocket costs should not be a barrier to having either one.
Clinical breast exam (CBE) and breast self-exam (BSE)
Research has not shown a clear benefit of regular physical breast exams done by either a health professional (clinical breast exams) or by women themselves (breast self-exams). There is very little evidence that these tests help find breast cancer early when women also get screening mammograms. Most often when breast cancer is detected because of symptoms (such as a lump in the breast), a woman discovers the symptom during usual activities such as bathing or dressing. Women should be familiar with how their breasts normally look and feel and should report any changes to a health care provider right away.
While the American Cancer Society does not recommend regular clinical breast exams or breast self-exams as part of a routine breast cancer screening schedule, this does not mean that these exams should never be done. In some situations, particularly for women at higher-than-average risk, for example, health care providers may still offer clinical breast exams, along with providing counseling about risk and early detection. And some women might still be more comfortable doing regular self-exams as a way to keep track of how their breasts look and feel. But it’s important to understand that there is very little evidence that doing these exams routinely is helpful for women at average risk of breast cancer.