For most women, the recommended age at which you should begin having annual mammograms is 40. However, there are many circumstances under which a woman would want or need to start having mammograms sooner. There is no danger in having an early mammogram; for some women, it can be a lifesaver.
If you’re under age 40, which is when it’s recommended that women begin having screening mammograms, you may think you are too young to get breast cancer—but that’s not true. While breast cancer in younger women is rare, it is the most common cancer among women ages 15 to 39. And certain kinds of breast cancer are on the rise among young women.
“While breast cancer is most typically diagnosed in post-menopausal women, this is a condition that can and does happen in young women, too,” says Yale Medicine radiologist Liva Andrejeva-Wright, MD, who specializes in breast imaging. “I have diagnosed women in their 20s with breast cancers.”
Overall, about 11% of all breast cancers occur in women younger than 45, according to the Centers for Disease Control and Prevention (CDC). An estimated 26,393 women under 45 are expected to be diagnosed with breast cancer this year. And every year, more than 1,000 women under age 40 die from breast cancer.
“While a majority of breast cancers that are found during annual breast cancer screening mammograms are in women over 50, women under 40 are generally too young to begin screening unless they have a mutation, a genetic reason or have physical symptoms, such as a mass or other breast changes,” explains breast oncologist Andrea Silber, MD.

Mammography
What is mammography?
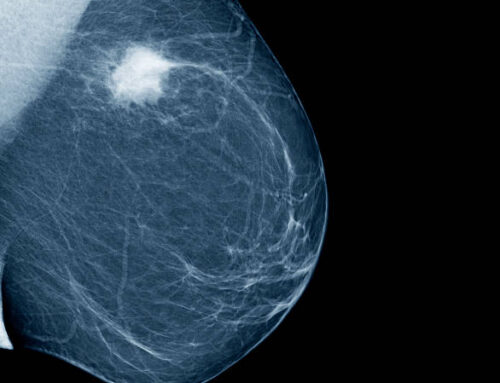
Mammography is an X-ray of the breast, which is performed by compressing the breast between an X-ray plate and a plastic plate. This spreads the breast tissue apart, helping ensure minimal movement and a sharper image.
There are two types of mammograms, “screening” or “diagnostic.” Screening mammograms are used to look for cancer in women who are symptom free. Diagnostic mammograms are those done on women who have lumps or other symptoms.
A mammogram is an X-ray image of your breasts. It can be used either for breast cancer screening or for diagnostic purposes, such as to investigate symptoms or unusual findings on another imaging test.
During a mammogram, your breasts are compressed between two firm surfaces to spread out the breast tissue. Then an X-ray captures black-and-white images that are displayed on a computer screen and examined for signs of cancer.
Mammograms play a key role in breast cancer screening. They can detect breast cancer before it causes signs and symptoms. Mammograms have been shown to reduce the risk of dying of breast cancer.
A traditional mammogram creates two-dimensional images of the breast. A newer type of mammogram called a 3D mammogram (breast tomosynthesis) creates three-dimensional images of the breast. Many medical facilities offer the 3D mammogram in addition to the traditional 2D mammogram for breast cancer screening.
Why it is done
Mammograms are X-ray images of your breasts designed to detect cancers and other changes in breast tissue. A mammogram can be used either for screening or for diagnostic purposes:
- Screening mammogram. A screening mammogram is used to detect breast changes that could be cancerous in people who have no signs or symptoms. The goal is to detect cancer when it’s small and treatment may be less invasive.Experts and medical organizations don’t agree on when to begin regular mammograms or how often the tests should be repeated. Talk with your health care provider about your risk factors, your preferences, and the benefits and risks of screening. Together, you can decide what screening mammography schedule is best for you.
- Diagnostic mammogram. A diagnostic mammogram is used to investigate suspicious breast changes, such as a new breast lump, breast pain, an unusual skin appearance, nipple thickening or nipple discharge. It’s also used to evaluate unexpected findings on a screening mammogram. A diagnostic mammogram includes additional mammogram images.
Why should you get a mammography?
Women in America have a 1 in 8 chance of developing breast cancer over their lifetime. Early detection offers the best hope for catching a cancer early when chances for a cure are highest. That’s especially important for African American women, who have a greater risk for some aggressive types of breast cancers and are more likely than white women to die from the disease.
“Breast cancer screening and early detection save lives,” says Alexander King, MD, Regional Director of Breast Radiology for RWJBarnabas Health Southern Region, which encompasses Monmouth Medical Center, Monmouth Medical Center Southern Campus and Community Medical Center. “Physician organizations agree that annual screening mammography, beginning at age 40, will save the most lives
One out of every eight women in the United States will get breast cancer, and it’s the second leading cause of death among women after lung cancer. If that’s not reason enough for getting mammogram, consider these reasons.
Family History
Women who have a family history of breast cancer should consider getting early mammograms. If your mother, grandmother, aunt, or sisters have had breast cancer, you should discuss it with your doctor and determine when the appropriate time to begin cancer screenings is. It may depend on the age at which your relative was diagnosed and what type of breast cancer they had.
BRCA-1 or BRCA-2 Gene
A small number of women discover with genetic testing that they have a mutated BRCA1 or BRCA2 gene. People with one of these mutated genes are at an extremely high risk of getting breast cancer. This gene mutation can be passed down to your children as well, which means you may have inherited it from a family member. If your family member was diagnosed with breast cancer at a young age, it’s possible they have the mutated gene. You should talk to your doctor about genetic testing and early mammograms.
A Lump in Your Breast
No matter your age, if you discover a lump in your breast during a monthly self-exam or any other time, you should consider getting a mammogram. Early detection and treatment are the key to surviving breast cancer. Never hesitate to talk to your physician or simply call us and make an appointment if you are concerned.
Having regular 3D mammograms performed by an experienced board-certified breast imaging specialist is the best way to detect abnormalities early. There is no appointment necessary; you can simply stop in at your convenience. You can also call (416) 759-3462 .
10 Reasons to Get a Mammogram Now :
- The risk of breast cancer increases significantly beginning at age 40 and continues to rise as you get older.
- Mammography has helped reduce breast cancer-related deaths in the U.S. by 30% since 1990.
- Mammograms find breast cancer on an average about 5 years earlier than you can feel it.
- Finding early-stage breast cancer allows more treatment options and a better opportunity for long-term survival.
- More than 3 out of every 4 women diagnosed (75-85%) have no family history or known risk factors of breast cancer. For this reason, mammography is a gold standard in cancer screening tests.
- Stamford Health’s Breast Center provides same-day results during business hours and performs additional imaging if needed.
- 3D mammograms detect breast cancer at an earlier stage with fewer false positives. 3D mammography has also improved our cancer detection rate by more than 50%.
- Connecticut has one of the highest rates of breast cancer in the country. This jarring fact is why our recommendations for breast cancer screening are slightly more proactive than those of some national organizations.
- Stamford Health is able to provide mammograms to anyone who is uninsured or whose insurance does not cover breast cancer screening, as long as you qualify. Ask your doctor.
- Stamford Health’s Breast Center was the first Accredited Center in the U.S. to be recognized by the National Accreditation Program for Breast Centers (NAPBC) and remains the only accredited program in the Stamford-Norwalk area. This level of excellence shows our commitment to your care.