Some people have a higher risk of developing breast cancer than the general population because other members of their family have had particular cancers. This is called a family history of cancer.
Having a mother, sister or daughter (first degree relative) diagnosed with breast cancer approximately doubles the risk of breast cancer. This risk is higher when more close relatives have breast cancer, or if a relative developed breast cancer under the age of 50. But most women who have a close relative with breast cancer will never develop it.
UK guidelines help GPs to identify people who might have an increased risk of cancer due to their family history.
Every woman has a one in eight chance of developing breast cancer in her lifetime. That’s a sobering statistic, but for women with a strong family history of this disease, the chance is even higher.
The good news is that when breast cancer is caught early, the five-year survival rate skyrockets to 92 percent. If you have close family members who’ve battled breast cancer, there are effective steps you can take to try to minimize your risk.

How Does Family History Play a Role in Breast Cancer Risk?
A woman is considered to be in the “high risk” category for developing breast cancer if she meets the following criteria:
- Has a first-degree family member (mother, sister, daughter or male counterpart) who’s had breast cancer.
- Has a parent or family member who’s tested positive for the BRCA1 or BRCA2 cancer gene.
- Has tested positive for the abnormal CHEK2 gene.
- Has received radiation treatment at a young age (10 to 30) for any chest condition.
If your mother or sister battled breast cancer, your chance of developing the disease is double. If more than one first-degree family member had the disease, your risk jumps fivefold. If you fall into any of these categories, you should talk to your doctor about proactive steps to reduce your cancer risk.
Breast cancer genes
If you have a very strong family history of certain cancers, there might be a faulty gene in your family that increases your risk of breast cancer. We know about several gene faults that can increase breast cancer risk and there are tests for some of them.
Genes that increase the risk of breast cancer are BRCA1 and BRCA2. Scientists are also looking at other genes that increase breast cancer risk.
Having one of these faulty genes means that you are more likely to get breast cancer than someone who doesn’t. But it is not a certainty.
Remember that most breast cancers happen by chance. Researchers estimate that only around 5 to 10 out of 100 breast cancers (5 to 10%) are caused by an inherited faulty gene.
Age of family member at breast cancer diagnosis
In general, the younger the relative was when she was diagnosed, the greater a woman’s chance of getting breast cancer.
For example, a woman whose mother was diagnosed with breast cancer before age 40 has about twice the risk of a woman without this family history. For a woman whose mother was diagnosed at an older age, the increase in risk isn’t as high.
Male family members with a history of cancer
History of breast cancer
People who have a close male relative (father, brother or uncle) who’s had breast cancer have an increased risk of breast cancer [32].
History of prostate cancer
People who have one or more first-degree relatives (father or brother) who’s had prostate cancer may have an increased risk of breast cancer, especially if the prostate cancer was diagnosed at a young age .
This increased risk is likely due to inherited gene mutations related to the risk of both breast and prostate cancers .
Inherited gene mutations
Families with a strong history of breast cancer often carry inherited gene mutations. Such families may have:
- More than one first-degree relative (mother, sister or daughter) with breast cancer
- A female relative diagnosed with breast cancer at an early age
- A male relative diagnosed with breast cancer at any age
- A family history of ovarian cancer
In the U.S., 5-10 percent of breast cancers are related to an inherited gene mutation .
Breast cancer screening for women with a strong family history of breast or ovarian cancer
There are special breast cancer screening guidelines for women with a strong family history of breast or ovarian cancer.
If you have a greater than 20 percent lifetime risk of breast cancer based mainly on your family history of breast or ovarian cancer, the National Comprehensive Cancer Network (NCCN) recommends you get a :
- Clinical breast exam every 6-12 months, but not before age 21
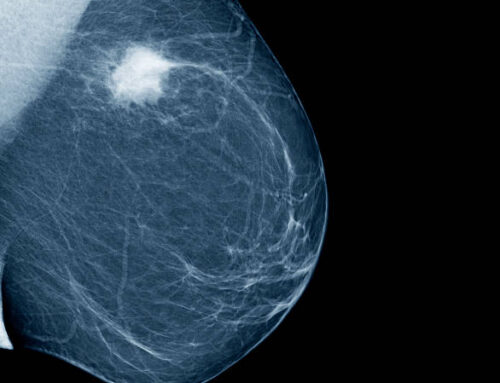
- Mammogram every year, starting at age 40 or starting 10 years younger than the youngest breast cancer case in your family (whichever comes first, but not starting before age 30)
- Breast MRI every year, starting at age 40 or starting 10 years younger than the youngest breast cancer case in your family (whichever comes first, but not starting before age 25)
Genetic testing
The NCCN recommends seeing a genetic counselor to discuss genetic testing if you have a family history of breast or ovarian cancer that may be due to an inherited gene mutation that increases the risk of these cancers .
The NCCN encourages genetic testing before getting a breast MRI as part of breast cancer screening. If you are found to have a BRCA1 or BRCA2 inherited gene mutation, or if you don’t wish to get testing, follow the recommendations above.
If testing finds you have a different inherited gene mutation related to breast cancer, it’s recommended you follow the screening guidelines for people with the specific gene mutation.
This medical care helps ensure if breast cancer does develop, it’s caught early when the chances of survival are highest.
Talking with your health care provider
If you have a family history of breast or other type of cancer, your health care provider can help you understand how this impacts your risk of breast cancer.
People with limited information on family medical history
You may not know your family medical history.
Risk assessment tools such as the Breast Cancer Risk Assessment Tool (Gail model) can estimate your breast cancer risk without this information. However, it will be less accurate without your family history details.
Talking with your health care provider about other risk factors for breast cancer can help you learn about your risk, even if you don’t have information on your family medical history.

How Mammograms Are an Effective Tool in Breast Cancer Detection
If you are at high risk for breast cancer, you need to develop a plan with your doctor for earlier and more frequent mammograms. Although yearly mammograms are usually not recommended until age 40, women at high risk should consider these additional screening strategies:
- Conducting a monthly self-exam of the breast
- Seeing a doctor or nurse practitioner for a yearly manual breast exam
- Receiving ultrasound screenings
- Getting MRI screenings
You and your doctor may decide on a plan that incorporates some or all of these strategies at different intervals. For example, you might get a yearly mammogram, but add an MRI or ultrasound every six months. You might also visit your doctor for a manual breast exam before following up with a mammogram. Your doctor will take your health history and risk factors into account to come up with the best plan for you.
What Are Other Ways to Lower My Chances of Getting Breast Cancer?
Following a healthy lifestyle can help lower your cancer risk. Some healthy choices you can make include:
- Losing weight
- Following a regular exercise program
- Cutting back on alcohol consumption
- Eating healthy foods including fruits and vegetables
- Stopping smoking
Referral to a specialist
Your GP will refer you to a specialist breast clinic or genetics clinic for assessment if you have any of the following:
- one first degree female relative diagnosed with breast cancer aged younger than 40 (a first degree relative is your parent, brother or sister, or your child)
- one first degree male relative diagnosed with breast cancer at any age
- one first degree relative with cancer in both breasts where the first cancer was diagnosed aged younger than 50
- two first degree relatives, or one first degree and one second degree relative, diagnosed with breast cancer at any age (second degree relatives are aunts, uncles, nephews, nieces, grandparents, and grandchildren)
- one first degree or second degree relative diagnosed with breast cancer at any age and one first degree or second degree relative diagnosed with ovarian cancer at any age (one of these should be a first degree relative)
- three first degree or second degree relatives diagnosed with breast cancer at any age
Your GP should also refer you if you have one first degree or second degree relative diagnosed with breast cancer when they were older than 40 years and one of the following:
- the cancer was in both breasts (bilateral)
- the cancer was in a man
- ovarian cancer
- Jewish ancestry
- sarcoma (cancer of the bone or soft tissue) in a relative younger than age 45 years
- a type of brain tumour called glioma or childhood adrenal cortical carcinomas
- complicated patterns of multiple cancers diagnosed at a young age
- two or more relatives with breast cancer on your father’s side of the family
Finding out your risk level
At the end of your appointment, if your specialist team has enough information, you’ll be told what your level of risk is based on your family history.
There are three possible levels of risk for breast cancer.
General population risk (average or near population risk)
General population risk means the risk of getting breast cancer is the same as, or very similar to, that of the general population.
One in seven women in the UK will develop breast cancer in their lifetime.
If only one person in your family has been diagnosed with breast cancer over the age of 40, you’re likely to be at general population risk.
Moderate risk (familial or raised risk)
People in this category are at higher risk than the general population. However, it’s still more likely they will not get breast cancer, despite their family history.
Someone at moderate risk may have several relatives with breast cancer but no obvious pattern of the disease. Although breast cancer might affect people in several generations of their family, they tend to be affected at older ages.
A person may also be considered at moderate risk if one close relative developed breast cancer under the age of 40.
High risk (hereditary or increased risk)
People in this category are more likely than those at moderate risk to develop breast cancer, but this does not mean they definitely will.
Someone at high risk will usually have had several close relatives on their mother’s or father’s side diagnosed with breast cancer, ovarian cancer or both over several generations (for example grandmother, mother and daughter). They will often have been diagnosed at a younger age, often under the age of 50.
What happens next?
For people at general population risk
If you’re told you’re at general population risk, you should be given information about routine breast screening. In the UK, women aged 50 to their 71st birthday are invited for a mammogram every three years.
You should also be told about the importance of being breast aware and reporting any possible signs of breast cancer.
It’s important to go back to your GP if your family history changes – for example if another relative develops breast or ovarian cancer.
For people at moderate risk
People at moderate risk are likely to be offered regular breast screening. Screening for woman at moderate risk is offered from the age of 40, which is earlier than routine breast screening.
Your specialist team may also discuss with you the possibility of drug treatments to reduce the risk of breast cancer.
You can read more about these options in our booklet Family history of breast cancer: managing your risk.
It’s important to go back to your GP if your family history changes, for example if another relative develops breast cancer or ovarian cancer.
For people at high risk
If you’re at high risk, you’ll be given information on the options available to you, including breast screening and risk-reducing surgery or drug treatments.
You can read more about these options in our booklet Family history of breast cancer: managing your risk.
You’ll be offered genetic counselling, and the possibility of genetic testing will be discussed.
Genetic counselling
If you’re considered to be at high risk of developing breast cancer, you’ll be offered a genetic counselling appointment at a regional genetics centre.
Genetic counselling can also be offered if you have an unusual family history or if further investigation into your family history would be helpful in understanding your risk.
You’ll meet with a genetic counsellor (a healthcare professional with specialist knowledge of genetics and inherited illnesses) or a clinical geneticist (a doctor with specialist training in genetics).
They can help you understand more about your family history and your risk of developing breast cancer and possibly other cancers.
They can also tell you about the options that may be available to you, such as:
- Genetic testing
- Breast screening
- Drug treatments to reduce the risk of cancer developing
- Surgery to reduce the risk of developing cancer
You can read more about these options in our booklet Family history of breast cancer: managing your risk.
This may be done over several visits.
For some people, genetic counselling can be a very emotional time.
You may feel anxious talking about your risk and what this means for you and those around you.
Your genetics team will have a lot of experience talking through the issues involved and will be able to offer you support if you need it.